Guidelines for treating patients with bipolar disorder
“Bipolar Disorder”, also known as”Bipolar Affective Disorder” — this disorder is closely related to mood.
It affects an estimated 60 million people worldwide, with a higher incidence among young people. The risk of suicide is more than 15 times that of the general population. Bipolar disorder may account for a quarter of all suicide deaths. So what can you do to help yourself if you or a loved one already has bipolar disorder?
How can people with bipolar disorder help themselves
Bipolar disorder is a mental illness, and having it can make you feel like your life is out of control. But there are practical ways you can improve and relieve your symptoms and improve your quality of life.
1. Know your emotional state
Monitor your emotions by:
You can use a mobile app to track your emotional state over time;
Identify the triggers that trigger your mood shift:
If you feel super excited after a late night or tend to get down on deadlines, you can avoid or minimize their impact on your mood by recognizing these patterns;
Know the telltale signs when your mood changes:
Every time you have a manic or depressive episode, there are bound to be some observable changes, such as changes in sleep, appetite, or behavior.

2 Take practical steps
Make a routine routine:
Include daily activities such as eating a healthy diet, getting enough sleep on time, and exercising regularly; Relaxation or mindfulness; Hobbies and social activities;
And taking medications at the same time each day, if any, to better avoid side effects and help your system stay stable.
Learn to handle stressful events and manage your finances
Be prepared for when a crisis happens:
You may need emergency support, such as the option of hospitalization, when you feel really bad, or when the manic, depressive episode lasts for a long time, or when conventional treatment fails.

3 Take advantage of social support networks
Learn to get help from your closest family or friends.
Join peer support groups:
Connecting with people who have been through similar experiences is an effective way to help you through difficult times by sharing your emotions, feelings, thoughts, etc.
If you are a close friend of the sufferer, what should you do?
How can you help someone with bipolar disorder
1. Keep an open mind
Listening to people with bipolar disorder talk about their experiences with an open mind will help them feel supported, accepted, and included.
2. Prepare yourself for manic episodes
While they are in their normal phase, try to ask what kind of help and support they need when they are in their manic/hypomanic episode.

3. When it comes to tricky situations, it’s best to communicate
You need to try to stay as calm as possible, not provoke or annoy them, and try to let them know that even if you can’t see or hear them, you can understand how they feel. It can be helpful to empathize by putting yourself in their shoes.
4. Identify the signs and triggers of their state transition
Most people have some symptoms that precede a manic or depressive episode. The best way to learn about these “signs” is to talk to them.
5. Try not to make excessive assumptions
In caring for someone with bipolar disorder, you can more or less observe some pattern of seizures, but not all mood changes will turn into extreme manic or depressive episodes, and don’t be overly sensitive or alert.

There are several types of bipolar disorder
In the current DSM diagnostic system, there are two main types of bipolar disorder: bipolar I disorder and bipolar II disorder.
A diagnosis of bipolar I disorder requires at least one manic episode and may also experience a major depressive episode, but is not necessary.
For bipolar II disorder, at least one hypomanic episode and one major depressive episode must have been experienced at the same time. The major difference is that if you have a manic episode, you must be diagnosed with bipolar I disorder.
There is also a rapid-cycling type of bipolar disorder, which is called rapid-cycling bipolar disorder if an individual has at least four mood episodes that meet the criteria for manic, hypomanic or major depressive episodes within a 12-month period.

There may be periods of lull between reverse-phase episodes, but there are also times when a person’s mood can change dramatically within a day or even an hour. Currently in the DSM system, this type is not separate, but listed as an adjunct.
It is important to note that rapid cycles can occur with any bipolar disorder.
In addition, individuals may be diagnosed with cyclothymic mood disorder if they have multiple hypomanic symptoms in at least 2 years, but do not meet the diagnostic criteria for hypomanic episodes, and multiple depressive symptoms, but do not meet the diagnostic criteria for major depressive episodes.
These symptoms are usually mild and can even become a way of life, especially for people who are engaged in creative work. During the hypomanic phase, they can work tirelessly and feel their ideas flowing and their inspiration erupting, and the disorder can even become a tool to help them work better.

Who’s prone to bipolar disorder
There is currently no very clear pathogenesis of bipolar disorder. There are five main causes of bipolar disorder that have been identified:
1. Childhood abuse
People who have experienced severe emotional trauma in childhood, such as sexual abuse, physical abuse, emotional neglect, traumatic events, and the loss of a loved one, are more likely to develop bipolar disorder as adults.
2. Stress life events
Acute stressful events such as the breakdown of an intimate relationship, money problems, and traumatic loss can be triggers for some symptoms, while being chronically stressed over a long period of time can equally lead to manic or depressive episodes.
3. Have self-esteem issues
When you are feeling very low, have very low self-esteem, or feel worthless, “manic” may become a coping style/defense mechanism that helps you regain your confidence.
4. Brain chemistry
Studies have found that some specific psychiatric medications can improve symptoms of bipolar disorder, and these medications typically act on neurotransmitters (chemical messengers) in the brain.
5 Genetic inheritance
Family history of bipolar disorder is the strongest and most consistent risk factor for bipolar disorder. The risk is 10 times greater in adult relatives of individuals with bipolar I disorder and bipolar II disorder than in the general population.

Manifestation of people with bipolar disorder
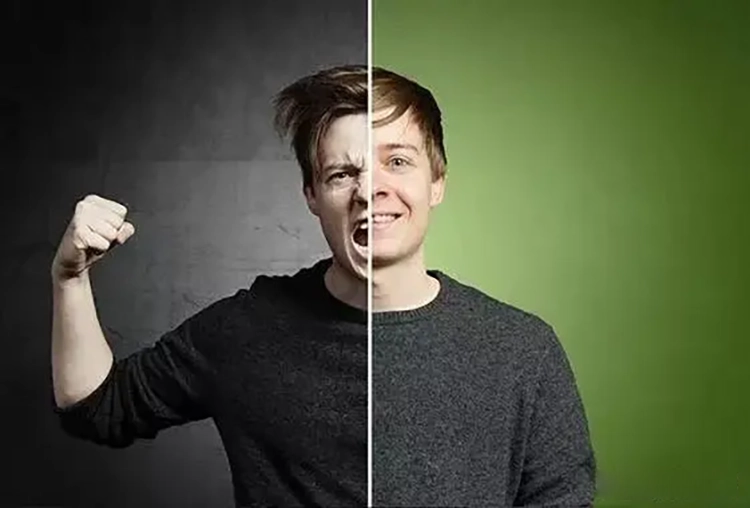
Everyone has emotional ups and downs, but for people with bipolar disorder, the emotional rollercoaster can be extreme: sometimes high and high; At other times, they’re pessimistic and down.
In addition to experiencing extreme changes in mood, people with bipolar disorder also experience dramatic changes in energy and behavior. These changes are called cyclical cycles.
They usually go through:
Manic or hypomanic episodes – high mood
Hyperdepressive episode – low mood
There may also be some underlying psychotic symptoms within the cycle of a manic or depressive episode
Bipolar disorder is a disorder in which both manic episodes and depressive episodes may occur.

“Bipolar” means that the person’s state fluctuates between two opposing phases, mania/hypomania and depression.
In a typical case, a person with bipolar disorder will have a manic episode, which may be followed by a normal lull, followed by a depressive episode, followed by another lull, and so on.
It may also be that a manic episode is followed by an antiphase episode, a depressive episode, with two or a pair of episodes followed by a lull.
1. Manifestations during manic episodes
Manic episodes are essentially characterized by well-defined periods of marked abnormal and persistent mood elevation, distension, or irritability, and sustained increased activity or energy for at least 1 week for most of almost every day.
A manic episode is usually characterized by euphoria, excessive pleasure, euphoria, or “feeling on top of the world.”
If more than 3 or 4 of the following symptoms are present, a manic episode is likely to be indicated:

Inflated or exaggerated self-esteem
You may grossly overestimate your abilities, think that you are the smartest, omnipotent, impervious to poison, and even hallucinate that you can hear things that others cannot. They may also make promises they cannot keep and believe they can complete an extremely complex task, such as writing a novel or creating an invention, when they know very little about it.
The need for sleep is reduced
This is different from insomnia, which is wanting to sleep or feeling the need to sleep but not being able to. When in a manic episode, it is possible to sleep for very little time, even as little as three hours a day, and feel rested and energized. In severe cases, you may go days without sleep and not feel fatigued.
Be more talkative than usual or feel pressured to keep talking
There may be a desire to keep talking quickly and communicate indiscriminately, even in an intrusive manner. If in an irritable state, rudeness or aggression may also occur.
Drifting thoughts or the subjective perception of a flight of thought
In conversation, you may jump from topic to topic quickly, even without any logic or organization. Sometimes you may feel like you have “too many brains”, or that you have so many ideas in your head that you can’t speak fast enough to express yourself.

Self-reported or observed situational transfers
Distraction or inability to concentrate may occur and is easily disturbed by external stimuli.
Increased goal-directed activity or psychomotor agitation
You may suddenly feel friendly, very interested in relationships or sexual relationships, constantly reaching out to old or casual friends or even strangers, but not taking into account that these interactions can seem intrusive, overbearing, and demanding.
Psychomotor agitation or restlessness, walking around, or holding multiple conversations at the same time may also be common.
Excessive involvement in high-risk activities that can have painful consequences
There may be shopping sprees, donating property, dangerous driving, foolish business investments, imprudent sexual behavior, drug or alcohol abuse, and even self-harm.
2. Behave during episodes of hypomania
Hypomania is similar to mania but is shorter in duration, typically lasting about four days, and does not exhibit the psychotic features of manic episodes, such as delusions, hallucinations, and self-injurious behavior. The impairment of social functioning is usually not significant and does not require hospitalization.

3 Manifestations during depressive episodes
Major depressive episodes typically last up to 2 weeks or more, and during this cycle, five or more of the following symptoms may be present:
Feelings of sadness, emptiness, hopelessness, or unexplained tears, crying (note: Children and adolescents may present as irritable moods).
Decreased interest and pleasure in activities.
Significant weight loss or gain; Or a loss or increase in appetite.
Insomnia or too much sleep.
Psychomotor agitation or retardation (fidgeting or becoming sluggish).
Fatigue or low energy. Excessive, inappropriate feelings of worthlessness and guilt (which can reach delusional levels).
Reduced ability to think, inability to concentrate, or indecision.
Recurrent thoughts of death (rather than just a fear of death), suicidal ideation without a specific plan, or some kind of suicide attempt, or a specific plan to carry it out.
There may also be mixed episodes, which correspond to the symptoms of both a manic episode and a depressive episode.
This is the worst case scenario, it’s more unpredictable and dangerous, it’s harder for the person to sort out what they’re feeling and what kind of help they need, two very different emotions at the same time, it’s harder for the individual to control and manage their emotions, and therefore more likely to commit suicide.

