How to tell if shortness of breath is from anxiety
How to tell if your shortness of breath is anxiety when you have trouble breathing? If you have this concern, then there are several things to consider:
1. Accompanied by other anxiety symptoms
2. Changes in breathing patterns
3. Situational factors
4. Duration
5. The effect of breathing training
6. Seek immediate medical attention

1. Accompanied by other symptoms of anxiety
Difficulty breathing due to anxiety is often accompanied by other anxiety symptoms such as heart palpitations, sweating, chest tightness, shaking, dizziness, or stomach upset.
These symptoms are commonly seen during acute episodes of anxiety, such as panic attacks. If these symptoms coincide with difficulty breathing and change rapidly over a short period of time, they may be related to anxiety.
Although the patient may experience feelings of choking or dying, these feelings, while real, are not malignant and are not life threatening.

2. Changes in breathing patterns
Anxiety often leads to rapid, superficial breathing (hyperventilation). During an anxiety attack, the person may suddenly experience shortness of breath, which can progress to dyspnea.
This dyspnea is a functional change that results from dysregulation of the autonomic nervous system. Difficulty in trying to breathe deeply may also indicate that difficulty breathing is related to anxiety.
3. Situational factors
Anxiety is often linked to specific situations or stressors. If difficulty breathing occurs in the face of a stressful, tense, or fearful situation, and the symptoms lessen or disappear when calm and relaxed, it may be related to anxiety.

4. Duration
Breathing difficulties caused by anxiety are usually short-lived and gradually ease after the acute phase until they disappear. Breathing difficulties may recur the next time an anxiety attack occurs.
Other potential physical causes should be considered if the breathing difficulty is prolonged or exists regardless of whether or not you are in an anxious state.
5. The effects of breathing training
Difficulty breathing during an anxiety attack usually responds well to methods such as deep breathing, relaxation techniques, or meditation. Going through these techniques can help relieve symptoms.

6. Seek immediate medical attention
Prompt medical attention is recommended if you suspect that your breathing difficulties are caused by anxiety. Use an anti-anxiety treatment regimen that can be effective in relieving symptoms or even making them disappear completely.
In addition, prompt medical attention can be used for a physical exam to rule out other possible causes such as asthma, lung disease, or heart problems.
Through the above several methods, we can better judge whether the breathing pain is caused by anxiety, but I think in addition to understanding these, we also need to have a certain understanding of breathing difficulties in order to better judge.

The definition and mechanism of dyspnea
Definition of dyspnea
Dyspnea (Dyspnea) In Greek, dys is the consciousness of pain and difficulty, while pneuma, means to breathe. Dyspnea is very common in chronic respiratory diseases and is the most urgent and painful of the many respiratory symptoms. Dyspnea at rest often indicates insufficient ventilation, while dyspnea with light activity often indicates a more serious condition. In respiratory rehabilitation, dyspnea is also one of the indicators often used to judge the intensity of activity and whether it can continue to be active in clinical rehabilitation.
Dyspnea is defined by the American thoracic society (ATS) in 1999 as the subjective experience of breathing discomfort, which is composed of a variety of different sensations of varying intensity. In this process, a variety of physiological, psychological, social and environmental factors interact with each other and may induce secondary physiological and behavioral reactions.

This definition states:
(1) Different sensations (such as exertion, tension, and lack of air/breathing) are involved in the formation of dyspnea through different pathways and mechanisms.
(2) Different sensations usually do not occur in isolation.
(3) The dyspnea sensation also has different unpleasant and emotional and behavioral manifestations.
It is emphasized here that dyspnea is a variety of feelings, and dyspnea is usually accompanied by emotional and behavioral abnormalities.
There are three main types of breathing discomfort sensations:
The first is a lack of air, in which the patient feels that the inhalation is not satisfied and needs more adequate breathing.
The second is an increase in the amount of work done in the breathing, and there is a feeling of exertion in the muscles when breathing.
The third is a feeling of tightness in the chest, which is often associated with bronchospasm and asthma-like sensations.
In addition, the depth and frequency of breathing can also be used to understand the feeling of difficulty breathing.

Mechanisms of dyspnea
Normal breathing control
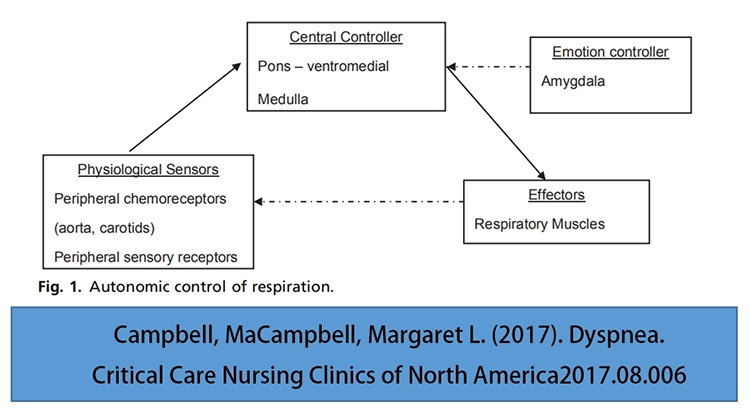
In functional magnetic resonance studies of spontaneous breathing in healthy people, it has been found that spontaneous breathing comes from conscious cortical control. The autonomic response is indeed regulated in the brain stem, which is fundamental and essential to the organism’s existence and will override conscious control. For a person who has difficulty breathing, it may be possible to get him to actively slow down his breathing.
Respiratory sensors consist of central (medulla, pons) and peripheral chemoreceptors (aorta and carotid bodies) and peripheral sensory receptors in the chest wall, airways, and lungs. Changes in respiratory function produce changes in blood gas imbalances (hypoxemia and hypercarburemia) and thoracic displacement. The peripheral afferent nerve plays only a minor role in respiratory contractions.

Stimulation of the respiratory center causes an increase in respiratory and cardiac responses by activating the parapontine complex, the sympathetic nervous system, and activating the adrenal medullary catecholamines (epinephrine and norepinephrine). The increased cardiac and lung response of the central respiratory control and sympathetic nervous system produces a compensatory response, including an acceleration of heart and respiratory rates, increased lung volume through recruitment of thoracic accessory muscles, changes in muscle tone, and an increase in mean arterial pressure. These cardiorespiratory responses are intended to restore respiratory homeostasis and sustain life.

Mechanisms of dyspnea
The activity of the respiratory muscles is controlled by the center of the brain, which sends orders to increase the contraction of the muscles. When the muscles are weak or hyperventilated, the degree of respiratory effort is further increased. This particular sense of effort is “inferred discharge” through the sensory cortical pathways sensed by the motor cortex and the brainstem respiratory neurons. Normally, the brain determines the need for ventilation through incoming information from the nervous system. When the muscular response is inconsistent with the incoming information received by the brain, this is known as “mismatch” or “neuronal ventilation separation” resulting in breathing difficulties.
Not all awareness of breathing is recognized by the brain as dyspnea. The brain filters out some of the sensations of breathing, allowing only some of them to reach the level of awareness, a function that keeps the brain from being flooded with constantly irrelevant information. The brain only “accesses” the sensation when it needs to.
There are mechanoreceptors in the muscles, tendons and neuromuscular junctions of the chest wall. When the lung capacity is limited, these mechanoreceptors transmit information to create different sensations of breathing. Stretching the chest wall relieves dyspnea, confirming the existence of this mechanism.
The incoming impulse of the lung vagus nerve receptor can stimulate the respiratory center and sensory cortex. Some studies have found that vagus nerve blocking can improve dyspnea during exercise and breath holding, suggesting that the vagus nerve is involved in the formation of dyspnea.
Clinical and experimental studies of dyspnea focus on dyspnea as a feeling, but it is not just a feeling, but mixed with the sensory and the corresponding biological psychological and social factors. Like pain, dyspnea is associated with emotional anxiety, unhappiness, panic, and depression. These symptoms aggravate the degree of difficulty breathing. Functional MRI studies in healthy subjects have shown that the anterior insular cortex and limbic structures are significantly activated in the presence of insufficient air (Figure 2).
References
[1] Respiratory rehabilitation Basics Tutorial. People’s Medical Publishing House, 1st edition, July 2019.
[2] Pulmonary Rehabilitation Success Guide. People’s Medical Publishing House. 1st edition, May 2019.
[3] Campbell, MaCampbell, Margaret L. (2017). Dyspnea. Critical Care Nursing Clinics of North America2017.08.006.
[4] Evans KC et al. Bold fMRI identififies limbic, paralimbic, and cerebellar activation during air hunger. J Neurophysiol 2002; 88:1500-1511.
[5] Parshall, Mark B et al . (2012). An Official American Thoracic Society Statement: Update on the Mechanisms, Assessment, and Management of Dyspnea. American Journal of Respiratory and Critical Care Medicine, 185(4), 435–452.

